An Introduction to the Katie Beckett Waiver in Tennessee
*Last updated 8/5/25
This article provides an overview of the KB waiver in TN. For updates to the program, see Key 2025 Changes.
The first Katie Beckett waiver was implemented in 1981 after President Ronald Reagan was inspired by the story of Katie Beckett. She was a young girl in Iowa who developed a brain infection when she was 5 months old, which led to her being paralyzed and spending three years in the hospital. After the hard work of many advocates, the Katie Beckett program launched in Tennessee in November 2020 and is available for ages 1-18.
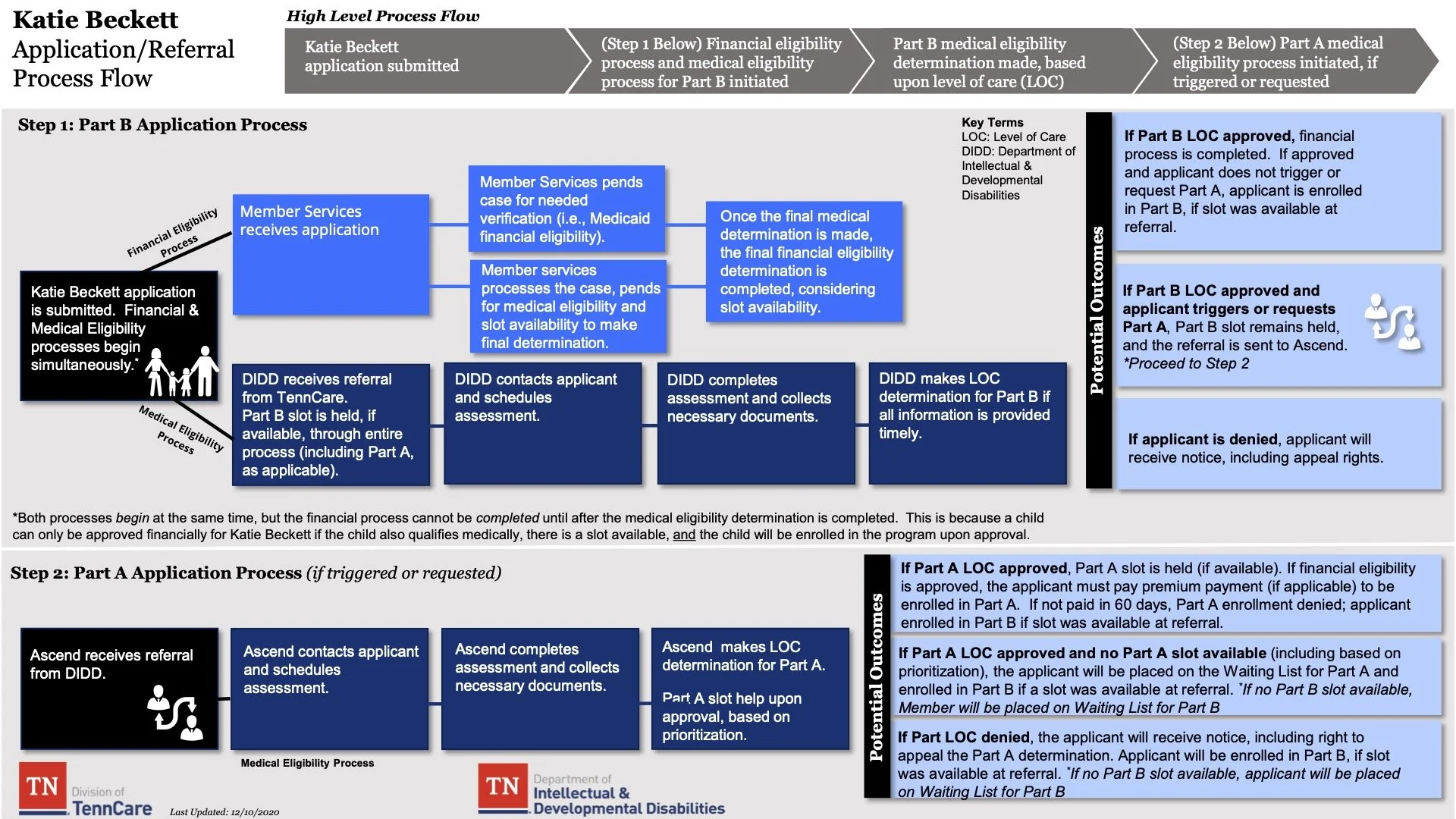
To apply for Katie Beckett, families must first go through a financial review and a medical review. The financial review will determine whether the child qualifies for Medicaid or the Katie Beckett waiver. The medical review helps determine what level of care the child needs.
When applying, families need to create a profile with self-referral at TennCare Connect. Creating this online is the fastest and easiest method; however, a DIDD case manager can help you complete the self-referral. To get help, call the DIDD office in your region:
West Tennessee Regional Office: (866) 372-5709
Middle Tennessee Regional Office: (800) 654-4839
East Tennessee Regional Office: (888) 531-9876
A DIDD case manager will be in contact to set up an assessment where medical documentation will be required regarding an individual's condition or disability. Proof will be required through these documents at the time of assessment, or applications can be denied or delayed.
This visual helps walk through the application process:
Children are grouped into 3 tiers. Tier 1 is for children with complex medical and behavioral needs. Tier 2 is for children who have complex needs, but their needs aren’t as high as Tier 1. These children can have medical, behavioral, or functional needs. Tier 1 will enroll in Part A. Other children can enroll for Part B while waiting. Part A receives $15,000/year and is enrolled in Medicaid. Part B receives $10,000/year.
There are a limited number of slots available in both Part A and Part B. Part A is based on the level of need, while Part B is on a first come first first-served basis. An individual can remain in the program until 18 if they continue to meet all qualifications.
There is a third tier, Part C, which is for children who currently have Medicaid, but their coverage is ending due to an increase in income or resources. If a child would qualify for Part A, but there is no available slot, this tier would allow them to keep their Medicaid coverage until a Part A slot opens. Individuals in Part C will NOT receive Home and Community-Based Services (HCBS).
What About Income Limits?
A common question families have is whether there are income limits for the Katie Beckett program. The important thing to know is that there is no income ceiling based on the parents’ income. Instead, eligibility is determined based on the child’s assets.
The program uses an asset ceiling that applies only to the child, not the parents. Unless the child has a significant amount of assets (such as a large savings account or an estate in their name), income and financial resources do not impact eligibility. This structure allows many families who might not qualify for other programs due to income to still receive support through Katie Beckett.
Billing Provider Changes for the Katie Beckett Program
The Katie Beckett program has undergone several changes in billing service providers over the last several years. In 2024, the program transitioned from PayFlex to Inspira, following PayFlex’s rebranding. Now, in 2025, the program made another transition — this time from Inspira to TASC, as a result of the State of Tennessee’s competitive bidding process. View more in-depth information regarding this change here.
Families have continued to use TASC’s debit card, online portal, and mobile app to manage their reimbursement accounts. With TASC, families have had the flexibility to purchase a variety of eligible physical items and services to support their child’s needs, including music therapy. Some purchases require a LOMN (letter of medical necessity) from a healthcare provider, while others do not. The TASC debit card can only be used at point-of-sale (POS) machines coded for medical, dental, or vision expenses, and pharmacy use may be restricted to the pharmacy register. As a result, most families have used TASC primarily as a reimbursement service.
Reimbursements typically take about two weeks to process. Payments are usually issued on a Friday and deposited by the following Monday. Families may also opt to receive reimbursement via check and must provide proof of receipt for all submitted charges.
There are a limited number of slots available in both Part A and Part B of the Katie Beckett program. Part A is based on level of need, while Part B is first-come, first-served. The current estimated waitlist time is 2–6 months.
Example Items/Services Not Covered
Property taxes
Washing machine
Care.com monthly membership fees
Monthly recurring medical fees
Disney tickets/out-of-state amusement parks, museums, etc.
Printer
Example Items/Services That Are Potentially Covered (Most Require a LOMN)
Wheelchair ramp
Specialized locks for doors/windows
Respite care
Service animal
Testing and evaluations
Speech devices
ASL courses
Homeschooling curriculum and supplies
Non-traditional therapies are covered under the Katie Beckett waiver. Supporting developmental challenges can often be effectively addressed through services like our specialized pediatric music therapy programs! A LOMN is needed for Music Therapy to be covered for reimbursement. The paperwork can be challenging to navigate, but we’re here to support you along the way. Music Therapy is not covered by insurance in Tennessee, which makes the Katie Beckett waiver a phenomenal assistance in obtaining these services.
Why Music Therapy Is a Valuable Use of Katie Beckett Funding
One of the greatest advantages of the Katie Beckett program is the ability to use funds for services and supports that aren’t typically covered by insurance, and Music Therapy is a prime example. Since Music Therapy is not reimbursable through private insurance in Tennessee, Katie Beckett provides essential access to this meaningful, evidence-based intervention.
While therapies like Occupational Therapy, Physical Therapy, Speech Therapy, and ABA are often covered by insurance, many families use Katie Beckett funding for the essential items and services listed above.
Because many important services fall outside the scope of insurance coverage, it’s crucial to be strategic about how Katie Beckett funds are used. We strongly encourage families to utilize insurance-billed providers for therapies that are covered whenever possible, preserving waiver dollars for non-covered services like Music Therapy. This approach helps you get the most value out of your funding while meeting your child’s unique and individualized needs.
Important Update on Funding and Reimbursement Changes
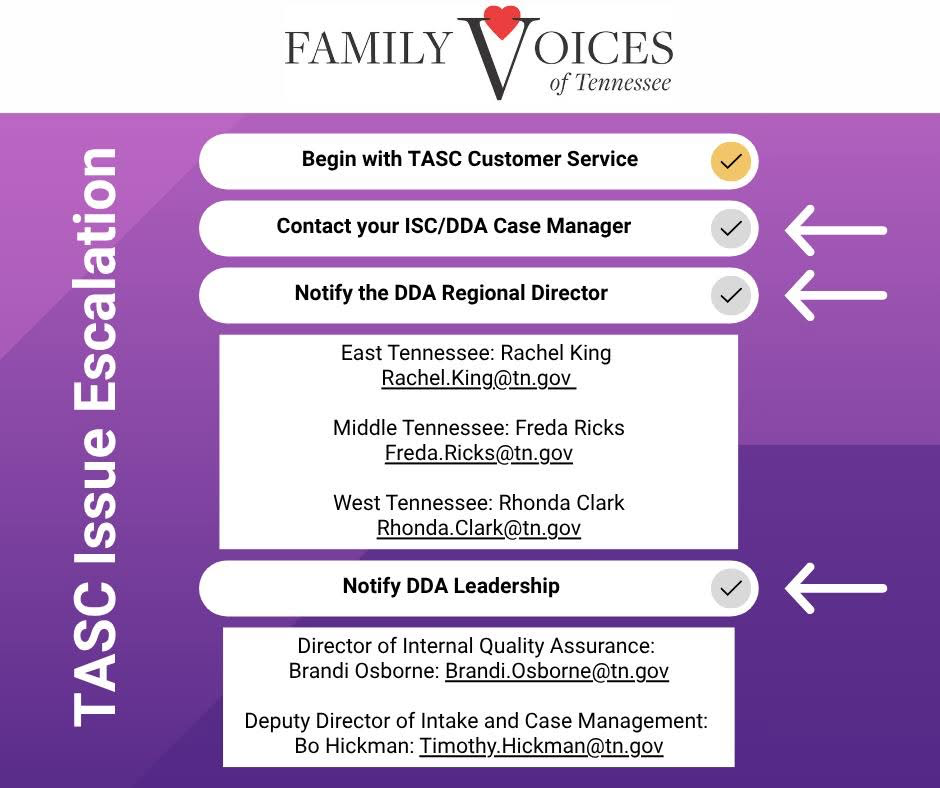
With the recent transition to TASC as the new company overseeing the Katie Beckett program, many families are experiencing challenges with the reimbursement process. This shift has brought a learning curve not only for families but also for TASC, as they adapt to managing the specific needs of this waiver program.
One of the biggest changes we’ve seen is an increased requirement for documentation. A Letter of Medical Necessity (LOMN) is now frequently required for nearly all purchases, whether it’s therapy services or everyday items like those from Walgreens. In addition, detailed, itemized receipts are being requested, and vague or general receipts are often denied.
As noted earlier, a LOMN is required for Music Therapy to be eligible for reimbursement. This now seems to apply across many types of services.
Musical Bridges has always provided detailed monthly invoices to our Katie Beckett families to help with the reimbursement process, and we’ll continue to do so. We know how valuable clear documentation can be, especially with the new expectations in place.
Explore inspiring success stories from Tennessee families who have benefited from using their Katie Beckett funds for music therapy.
Helpful Links:
DIDD Katie Beckett Page:
TennCare Katie Beckett Page:
Part A - https://youtu.be/0AJFjwHC-Fg
Part B - https://youtu.be/HbQ7lM8gr0U
While this is just a very brief overview, you can find more information about the Katie Beckett Program on both the DIDD and TennCare websites. Musical Bridges has many clients successfully enrolled in the program who are thriving in Music Therapy. If you have any questions about how your child can benefit from Music Therapy, please contact us to explore the benefits of our music therapy services for children with complex needs!